HepaLife is developing a bioartificial liver device intended for the treatment of liver failure using stem cells. The artificial liver, currently under development, is designed to serve as a supportive device, either allowing the liver to regenerate upon acute liver failure, or to bridge the patient's liver functions until a transplant is available. It is only made possible by the fact that it uses real liver cells, and even then, it is not a permanent substitute for a liver.
On the other hand, Researchers Dr. Colin McGucklin, Professor of Regenerative Medicine at Newcastle University, and Dr. Nico Forraz, Senior Research Associate and Clinical Sciences Business Manager at Newcastle University, say that pieces of artificial liver could be used to repair livers injured in the next five years. These artificial livers could also be used outside the body in a manner analogous to the dialysis process used to keep alive patients whose kidneys have failed.Here is a brief summary of the liver’s functions, but remember there are more than 500 functions: 1-processing digested food from the intestine, 2-controlling levels of fats, amino acids and glucose in the blood, 3-clearing the blood of infections, 4-neutralises and destroys toxins 5-produces bile, 6-storing iron, vitamins and other chemicals, 7-breaks down food and turns it into energy, 8-manufactures, breaks down and regulates hormones, 9-making enzymes and proteins.
Wednesday, July 14, 2010
Liver transplantation:
Human liver transplants were first performed by Thomas Starzl in the United States and Roy Calne in Cambridge, England in 1963 and 1965, respectively.
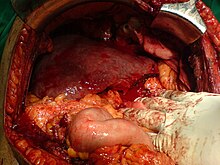
Liver transplantation is the only option for those with irreversible liver failure. Most transplants are done for chronic liver diseases leading to cirrhosis, such as chronic hepatitis C, alcoholism, autoimmune hepatitis, and many others. Less commonly, liver transplantation is done for fulminant hepatic failure, in which liver failure occurs over days to weeks.
Liver allografts for transplant usually come from non-living donors who have died from fatal brain injury. Living donor liver transplantation is a technique in which a portion of a living person's liver is removed and used to replace the entire liver of the recipient. This was first performed in 1989 for pediatric liver transplantation. Only 20% of an adult's liver (Couinaud segments 2 and 3) is needed to serve as a liver allograft for an infant or small child.
More recently, adult-to-adult liver transplantation has been done using the donor's right hepatic lobe which amounts to 60% of the liver. Due to the ability of the liver to regenerate, both the donor and recipient end up with normal liver function if all goes well. This procedure is more controversial as it entails performing a much larger operation on the donor, and indeed there have been at least 2 donor deaths out of the first several hundred cases. A recent publication has addressed the problem of donor mortality, and at least 14 cases have been found.[16] The risk of postoperative complications (and death) is far greater in right-sided operations than that in left-sided operations.
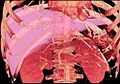
With the recent advances of non-invasive imaging, living liver donors usually have to undergo imaging examinations for liver anatomy to decide if the anatomy is feasible for donation. The evaluation is usually performed by multi-detector row computed tomography (MDCT) and magnetic resonance imaging (MRI). MDCT is good in vascular anatomy and volumetry. MRI is used for biliary tree anatomy. Donors with very unusual vascular anatomy, which makes them unsuitable for donation, could be screened out to avoid unnecessary operations.
Diagnosis and Biopsy:
Diagnosis:
The diagnosis of liver function is made by blood tests. Liver function tests can readily pinpoint the extent of liver damage. If infection is suspected, then other serological tests are done. Sometimes one may require an ultrasound or a CT scan to image the liver.
Physical exam of the liver is not accurate in determining the extent of liver damage. Physical exam can only reveal presence of tenderness or size of liver but in all cases some type of radiological study is required to look at the liver.Biopsy:
The ideal way to look at damage to the liver is with a biopsy. A biopsy is not required in all cases but may be necessary when the cause is unknown. The procedure is done at the bedside and only requires local anesthetic. A small thin needle is inserted into the skin just below the rib cage and a biopsy is obtained. The tissue is sent to the laboratory where it is analyzed under a microscope. Sometimes the radiologist may perform a liver biopsy under ultrasound guidance if only a small area is involved.
Disease signs:
The classic signs of liver damage include the following:
- Pale stools occur when stercobilin, a brown pigment, is absent from the stool. Stercobilin is derived from bilirubin metabolites produced in the liver.
- Dark urine occurs when bilirubin mixes with urine
- Bilirubin when it deposits in skin, causes an intense itch. Itching is the most common complaint by people who have liver failure. Often this itch cannot be relieved by drugs.
- Swelling of the abdomen, ankles and feet occurs because the liver fails to make albumin.
- Excessive fatigue occurs from a generalized loss of nutrients, minerals and vitamins.
- Bruising and easy bleeding are other features of liver disease. The liver makes substances which help prevent bleeding. When liver damage occurs, these substances are no longer present and severe bleeding can occur.
Liver Disease:
The liver supports almost every organ in the body and is vital for survival. Because of its strategic location and multidimensional functions, the liver is also prone to many diseases.
The most common include: Infections such as hepatitis A, B, C, E, alcohol damage, fatty liver, cirrhosis, cancer, drug damage (especially acetaminophen, cancer drugs)
Many diseases of the liver are accompanied by jaundice caused by increased levels of bilirubin in the system. The bilirubin results from the breakup of the haemoglobin of dead red blood cells; normally, the liver removes bilirubin from the blood and excretes it through bile.
There are also many pediatric liver diseases including biliary atresia, alpha-1 antitrypsin deficiency, alagille syndrome, progressive familial intrahepatic cholestasis, and Langerhans cell histiocytosis, to name but a few.
Diseases that interfere with liver function will lead to derangement of these processes. However, the liver has a great capacity to regenerate and has a large reserve capacity. In most cases, the liver only produces symptoms after extensive damage.
Liver diseases may be diagnosed by liver function tests, for example, by production of acute phase proteins.
Other fuctions of liver:
The liver manufactures plasma proteins from dietary amino acids.These proteins include albumins,globulins and those essentials for clotting of blood like fibrinogen.
Iron storage:
The red blood cells of the body become worn out after some time.These cells are not nucleated and are destroyed in the spleen and their haemoglobin is brought to the liver.The liver breaks down the haemoglobin and stores the iron released in the process.Bile pigments are also formed from the breakdown of the haemoglobin.
Detoxification:
Harmful substances may be absorbed into the blood stream from the gut.These substances(e.g. benzoic acid,picric and chloroform) are made harmless by the liver cells.The process of converting harmful substances into harmless is known as detoxification.Alcohol is also broken down in the liver.
Heat Production:
Heat is produced as a result of numerous chemical activites occuring in the liver.This heat is distributed by the blood to the other parts of the body,thus helping to maintain the body temperature.
Others:
Removals of hormones, toxins, etc. The liver extracts many harmful materials from the blood and excretes them in the bile or from the kidneys.
Formation of red blood cells in the young embryo while it is developing in the womb.
Making heparin: this is a substance that prevents the blood from clotting as it travels through the blood system.
Removal of hemoglobin molecules: when red blood cells die, the hemoglobin is converted into bile pigments and the iron atoms are saved for future use.
Storage of blood: the liver can swell to hold huge amounts of blood which can be released into the circulation if the body suddenly needs more, e.g. if it is wounded.
Forms plasma proteins: the plasma proteins are used in blood clotting and in keeping the blood plasma constant. The main blood proteins include fibrinogen, prothrombin, albumens and globulins.
Storage of vitamins such as vitamin A and D. Vitamin A is also made in the liver from carotene, the orange-red pigment in plants. Vitamin B12 is also stored in the liver.
Tuesday, July 13, 2010
What happens to the sugar in the liver?
When there is an exessive amount of glucose in the liver pancrease secretes more insulin(which will enter the liver) to store glucose by converting it to glycogen.The blood glucose level falls.
When there is too little amount of glucose in the blood,pancrease produces more glycerol to convert the stored glucose(glycogen) to glucose in the liver.The blood glucose level rises.
Oxidation of FATS in the liver:
Fats,before they are used,are brought to the liver where they are converted to to forms that can be oxidized or stored.Under normal conditions when there is an adequate supply of glucose,fats are not oxidized.They are used to build protoplasm,for example,in cell membranes.Exess fats are stored in special tissues called ADIPOSE TISSUE(for storage and insulating tissues) which occur beneath the skinb,around the heart,the kidneys and in the mesenteries binding the intestines.
Under certain,circumstances,foe example,in fasting,when there is an inadequate supply of glucose,the fats are oxidized to provide the energy foe the vital activites of the body.
Posted by Samama Shahid at 5:27 AM 0 comments
What happens to the Amino Acids in the liver?
Both sugars and amino acids must pass through the liver before they reach the general blood circulation.The routes for their transport are the same.
Amino acids which enter the cells are converted into new protoplasm and are used for growth and repair of worn-out parts of the body.They are also used for the formation of enzymes and hormones.
What does the liver secrete?


The liver is the largest organ in the body.It is dark red in colour and is made up of five lobes(a somewhat rounded subdivision of a bodily
 organ or part),three on the right and two on the left.Its upper surface touches the
organ or part),three on the right and two on the left.Its upper surface touches the  diaphragm and the lowest surface is in contact with the stomach and the small intestine.Attached to the lower surface of the liver are the three blood vessels,THE HEPATIC PORTAL VEIN,THE HEPATIC VEIN and THE HEPATIC ARTERY.
diaphragm and the lowest surface is in contact with the stomach and the small intestine.Attached to the lower surface of the liver are the three blood vessels,THE HEPATIC PORTAL VEIN,THE HEPATIC VEIN and THE HEPATIC ARTERY.